The Glasgow Coma Scale - A guide to Neurological Functioning
Anyone who has been posted in trauma or Orthopedics can tell you that the sound of an ambulance driving up to the entrance of the emergency, the tell tale squeaking of a rolling stretcher, and the wheeling in of a patient, is haunting. The air is tense. You walk up to the patient. A man around forty years of age lies there unresponsive - his hair disheveled and caked with blood.
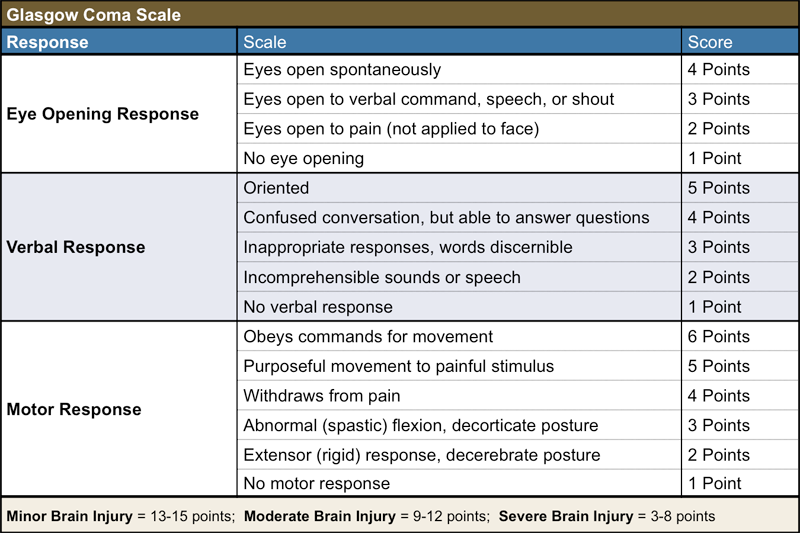
You ask the people who are with him about what happened and found out that he has suffered a trauma to his head. As you talk to the family, you pick up on him making noises. His speech is incomprehensible. On painful stimuli, you notice that he doesn't open his eyes, and that he flexes his limbs.
You stabilize the patient and ensure his vitals are within normal limits. What next?
Whether you’re an intern, a medical officer or the on duty neurosurgeon, the next step in evaluating the patient remains the same- assessment of the Glasgow Coma Scale (GCS). It goes without saying that the GCS must be monitored in all neurologically deranged patients.
The Glasgow Coma Scale is mandatory in assessing the level of consciousness of patients; it is essentially the gold standard for assessment of acutely ill patients with CNS insults. By serial charting of the GCS of a patient, we can assess trends in worsening or improvement and appropriately taper or escalate therapeutics, especially in the acute stages of illness.
The idea is that the GCS provides a simple, quick and effective insight into the patients neurological functioning and serves as a model to plot progression or regression of a neurological disease.
The Glasgow Coma Scale (GCS) was developed by Graham Teasdale and Bryan Jennet in 1974 to assess the level of consciousness in acute brain injury. Before the GCS we currently use came to be, during World War II, consciousness in head injury was described by psychological terminology- coma, semicoma, confusion (mild, moderate, severe), stupor, automatism, etc. The need for such a glossary of terms was to enable facilitation of information exchange between medical officers as the injured were transferred from station to station.
However, the problem with these terms was that they were subjective and not much could be inferred from them. I mean, how do you exactly define moderate confusion? What may be a confused man to one doctor may be a man in semicoma. There were simply too many discrepancies in such a system, and thus people quickly gave up on this system and began looking elsewhere for a more objective system of classification.
This need for an objective system was further exacerbated by neurosurgeons and intensivists who dealt with brain injury day in and day out. They were in desperate need of a clinical system that could help them understand the the progress of their patients.
In 1970, researchers in Glasgow, along with those in the Netherlands and the United States developed a tool to evaluate head injuries. As the data was to be interpreted using computers, the ultimate analysis was to convert clinical signs into numbers. A multidimensional approach assessing more than one system at a time using clearly defined terms led to the publication of what is now known as the Glasgow Coma Scale in 1974.
The GCS aimed to be a tool that observers of all levels of education could use in the medical field- nurses, doctors and students. It was developed not as a definitive predictor of prognosis, but as an adjunctive tool along with other forms of neurological assessment. Serial assessments of the GCS help modify treatment plans for current patients and allow us to study progression of diseases for future use.
The scale was promoted by the Advanced Trauma and Life Support, first edition, in 1980 and again in 1988 for the grading of subarachnoid hemorrhage by the World Federation of Neurosurgical Societies. In 2001, it was found that that the GCS is used by medical personnel in more than 80 countries worldwide and has been translated into the national language in almost all of them.
Despite how widely used the GCS is, it is not without its own weaknesses. Inability to predict outcome, variation among observers and loss of information after converting to numerical scale (as there can be any number of permutations among E, V and M for a given total GCS) are among such minuses. Since then, there have been several modifications of the GCS, for example, to suit the pediatric population and scales based off of the GCS, such the FOUR scale (full outcome of unresponsiveness). (J & C.)
The invention of the GCS points of a very important trend in then evolution of medicine - the importance of grading. The strength of western medicine lies in the fact that it is able to generalise subjective things into objective gradings in order to provide blanket treatment to a majority of populations. Now, obviously such a generalisation has it pros and cons, but in this instance, it has helped neurologists world over to act effectively in emergency situations.
Author: Shruthi Sivakumar
Sources and citations
1)Teasdale, Graham. “The Glasgow Structured Approach to Assessment of the Glasgow Coma Scale.” What Is GCS - Glasgow Coma Scale, www.glasgowcomascale.org/what-is-gcs/#adoption-and-spread.
2)Jennett, Bryan. “Development of Glasgow Coma and Outcome Scales.” Nepal Journal of Neuroscience, vol. 2, 2005, www.cmp-manual.cz/skaly/gcs/jennett_gcs.pdf.