Hypertensive Retinopathy - The Stealthy Blindness
Hypertension is defined as systolic blood pressure over 140mmHg or diastolic blood pressure greater than or equal to 90mmHg. (1)
The prevalence of retinopathy in hypertensives ranges from 6.6 to 17.2%. (2)
The arteriosclerotic changes of hypertensive retinopathy are caused by chronically elevated blood pressure.
Pathophysiology:
The pathophysiology of the disease is divided into 3 phases:
Vasoconstrictive phase:
This is an early phase where the rise in blood pressure leads the normally pliable retinal vessels to increase their tone.
It presents in patients as generalised arteriolar narrowing. (3)
When the blood pressure is continuously elevated, the intima of the blood vessels becomes thicker, there is hyperplasia of the media wall and hyaline degenration.
Sclerotic Stage:
In this stage, the generalised narrowing becomes more focal in nature and more areas are involved.
A commonly seen sign in this stage is A-V nicking, which occurs because of the arterioles compressing the venules at their junctions as they share a common adventitial sheath.
Thickening of arteriolar walls occurs in chronic hypertension leading to copper and silver wiring of vessels. (4)
Copper wiring is when arterioles with moderate vascular changes show a reddish-brown appearance.
Silver wiring occurs when there is severe vascular wall hyperplasia and thickening giving a more silver reflection.
Exudative Phase:
This is associated with an acute increase in the blood pressure.
Because of this, the blood retinal barrier is disrupted which leads to exudation of blood and lipids and retinal ischemia.
Other findings in this stage is the presence of flame-shaped hemorrhages, blot hemorrhages, hard exudates and cotton wool spots.
Image credit: Dr. Madhuvanthi Mohan
For more such ophthalmology related images and content, visit Ophthalmobytes on Instagrm.
What is seen in Chronic hypertensive damage?
Generalized arteriolar narrowing and arteriovenous nicking is usually seen in chronic hypertensive damage and may not correspond to the current blood pressure of the patient. (5)
There are many classifications for Hypertensive Retinopathy but one of the most common ones which every post graduate student should know is the one below.
Keith-Wagener-Barker Classification (6)
Grade 1: Generalised arteriolar narrowing.
Grade 2: Focal narrowing and arteriovenous changes.
Grade 3: Grade 2+ Hard exudates, flame shaped hemorrhages and cotton wool spots.
Grade 4: Grade 3+ Optic disc swelling.
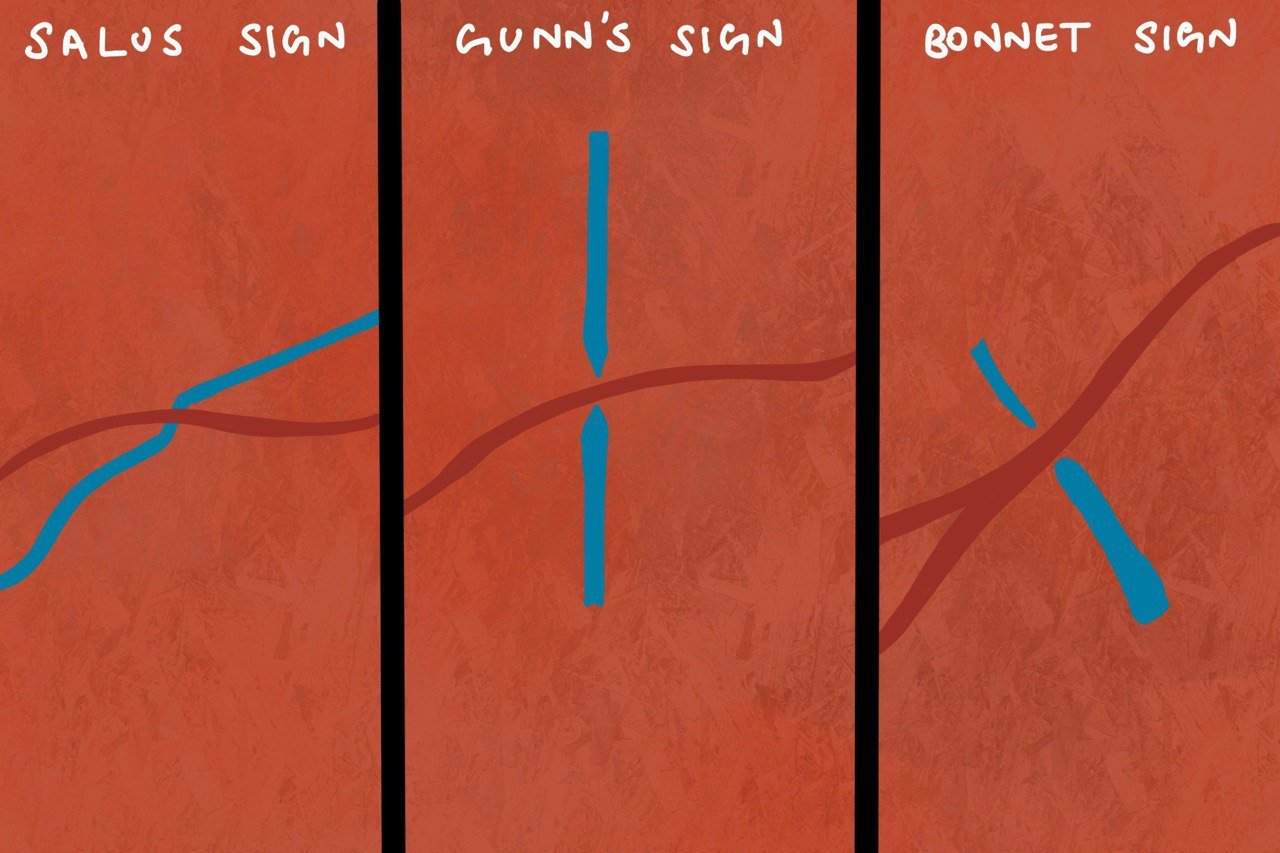
When we talk about Arteriovenous (A-V) crossing changes, we think of 3 signs:
Salus sign: Deflection of retinal vein as it crosses the arteriole.
Gunn's sign: Tapering of retinal vein on either side of the AV crossing.
Bonnet sign: Banking of retinal vein distal to the AV crossing
Image credit: Dr. Madhuvanthi Mohan
For more such ophthalmology related images and content, visit Ophthalmobytes on Instagrm.
Diagnosis:
Hypertensive retinopathy is a clinical diagnosis made with the characteristic vascular changes seen on the retina with the help of Indirect Ophthalmoscopy.
Treatment:
Main treatment for a patient with hypertensive retinopathy is to control the blood pressure. So in this case, an immediate referral to a physician is necessary for further management.
Early diagnosis of hypertensive retinopathy is extremely important as it is also a risk factor for clinical stroke, cognitive decline and cardiovascular mortality. (7)
Author: Madhuvanthi Mohan and Sashwanthi Mohan
## Sources and citations
1) Yoon SS, Carroll MD, Fryar CD. Hypertension prevalence and control among adults: United States, 2011-2014. NCHS Data Brief. 2015;(220):1-8.
2) Klein R, Klein BE, Moss SE, et al. Hypertension and retinopathy, arteriolar narrowing, and arteriovenous nicking in a population. Arch Ophthalmol 1994;122(1):92-8.
3) Wong TY. Fred hollows lecture: hypertensive retinopathy – a journey from fundoscopy to digital imaging. Clin Exp Ophthalmol. 2006;34(5):397-400.
4) Wong TY, Mitchell P. Hypertensive retinopathy. N Engl J Med 2004;351(22):231-2317.
5) Wong TY, Mitchell P. The eye in hypertension. Lancet 2007;369(9559):425-35.
6) Fraser-Bell S, Symes R, Vaze A. Hypertensive eye disease: a review. Clin Exp Ophthalmol. 2017;45(1):45-53.
7) Wong TY, Klein R, Nieto FJ, et al. Retinal microvascular abnormalities and 10-year cardiovascular mortality: a population-based case-control study. Ophthalmology 2003;110(5):933-40.