Acute Coronary Syndrome (ACS) - The importance of quick decisions
You’re the medical officer at an under staffed, over-worked Emergency Medicine department of a hospital. Obviously sleep deprived. It’s been a long 48 hour shift; you’re just about done, when as luck would have it, you have 3 cases wheeled in, waiting for you on three different examination couches.
You take a closer look, and all 3 are middle aged gentlemen, who have come with chest pain; all with chest pain at rest, the first with pain radiating to the jaw, the second to the left arm and the third with non specific features; there was a difference in the duration of the symptoms and how the pain was described by each. Further inquiry reveals a rather obscure heart disease history, and all 3 of them report occasional smoking and social alcohol consumption.
This is a fairly common presentation; though getting 3 cases at the same time seems highly unfortunate, the specific diagnoses of these types of patients isn’t really something to worry about; the management and their individual prognosis, however, is a completely different story. But in this article, we are going to understand about a clinical spectrum, called “Acute Coronary Syndrome (ACS)”, and how quick thinking can save lives, time, and a significant portion of the patient's heart muscle.
After a quick history, we do the physical examination. The patients are anxious, sweating profusely, have an elevated heart rate. Though quite unremarkable, this is how many of patients with ACS present; and this doesn’t give us any grounds to skip the physical examination, as it can give us possible clues to refute or consider alternate diagnoses.
The first and foremost investigation in any patient, who has come with a history of chest pain, is a 12-lead electrocardiogram (ECG). The ECG gives a good idea of how the electrical activity of the heart is; which by years of its interpretation, have come to stand for many underlying conditions of the heart.
Along with an ECG in the above 3 patients, we also need to do a cardiac troponin levels, which is a marker of cardiac myocyte injury.
With just these 2 investigations, we can differentiate between the three acute coronary syndromes:
- The Unstable Angina
- The Non-ST elevation Myocardial Infarction (NSTEMI)
- The ST-elevation Myocardial Infarction (STEMI)
So now, we have three possible diagnoses, and 2 investigations.
Let’s cut to some basics.
All these three conditions are coronary artery diseases, meaning that there is some block in the coronary arteries supplying the heart muscles. This produces a demand-supply mismatch and leads to hypoxia of the cardiac muscle, which manifests as pain.
The block is usually caused by an atheromatous plaque, which basically is all the cheese burst pizzas, and lack of exercise that decide to sign a treaty with the platelets and go and sit inside many vessels in our body, like the coronary arteries, and narrow the diameter of the vessel, thus reducing the amount of blood flowing to the area it supplies.
At rest, this seems to be an “okay” scenario. But on activity, there is some deficit, and this manifests as chest pain, or “angina”; when this pain disappears on resting, it’s called “Stable Angina”.
In ACS, the static obstruction to the blood flow, becomes dynamic and the flow goes below a critical level; hence, these patients have what is called “Angina at rest”, which is an ominous symptom.
If we recall, the 3 patients have come with this precise complaint, and we have done an ECG and a cardiac troponin level in each of them.
Now we might ask. How do the two investigations correlate to the pathology at hand?
When a cell is injured, and the injury provoking stimulus is not removed in time, the cell dies; and when it dies, all the stuff that’s inside the cells come out. After many years of research, we have found a particular substance that is ALMOST specific to the cardiac muscle cells, and they are the Troponin-C, Troponin-I and the Troponin-T, and of all 3, Troponin-I is fairly specific to the heart muscle. So when the heart muscles are damaged, these cardiac troponins go through the roof. We need to remember here that if the patient presents to us too early, the cardiac troponin levels may not be significantly high enough; the levels are reassessed after a few hours.
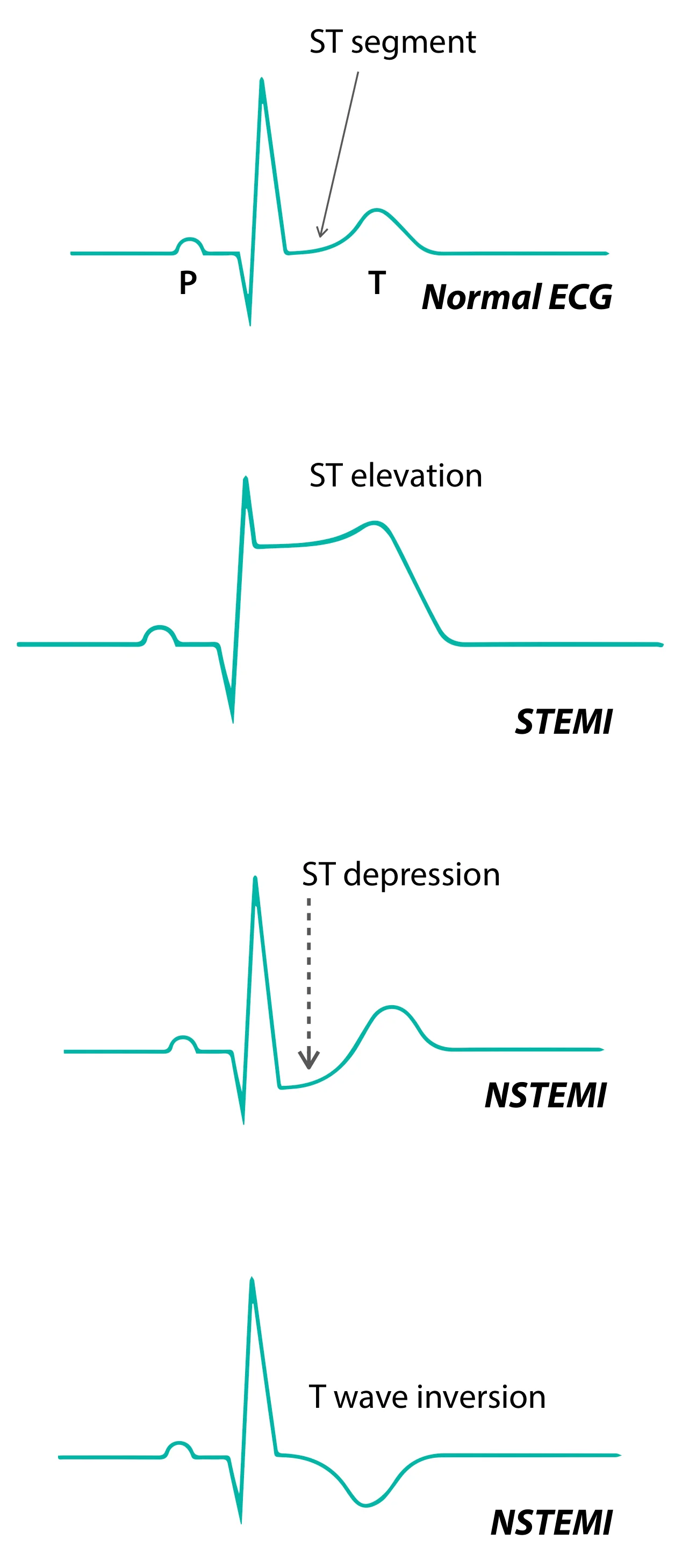
Next comes the ECG. The ECG is about pattern recognition, the basics of which require articles of its own, but to differentiate between the various types of ACS, we need to know about the ST-segment.
The ST-segment, between the end of the S-wave and the start of the T-wave, is iso-electric in a normal heart; meaning, that there is no electrical impulse conduction during that time, and the ST-segment assumes importance in our current scenario.
In the first patient’s ECG, there is an elevation of the ST-segments in many of his leads with appropriate changes (called reciprocal changes) in the other leads. With the typical history and his ECG changes, and elevated cardiac biomarkers to corroborate, a diagnosis of Acute ST-elevation Myocardial Infarction is made, and based on his time of presentation and the area of myocardium infarcted, a decision to take the patient up for percutaneous coronary intervention (PCI) or thrombolysis is made and further managed.
The other two, have ST-segment depression with or without T-wave inversion; this is when we know there’s either a possibility of NSTEMI or Unstable Angina. If there is evidence of cardiac myocyte death (as signified by elevated cardiac troponins), that is a case of NSTEMI, and if the levels aren’t elevated, then the diagnosis is most probably an Unstable Angina; these patients need invariably need medical therapy with anti-platelets, lipid lowering agents, lifestyle modification and regular follow-up.
So each of the three patients you saw right before you left, get a diagnosis within minutes and get their lives saved; and you get to go home, tired, but satisfied.
Author: Anirudh Murali (Facebook)
Sources and citations
Cannon, Christopher P., and Eugene Braunwald. “Chapter- 294: Non-ST Segment Elevation Acute Coronary Syndromes.” Harrison's Principles of Internal Medicine, 19th ed., McGraw-Hill Education, 2015, pp. 1593–1596.
Antman, Elliot M., and Joseph Loscalzo. “Chapter- 295: ST- Segment Elevation Myocardial Infarction.” Harrison's Principles of Internal Medicine, 19th ed., McGraw- Hill Education, 2015, pp. 1599–1602.